By Alana Tang
Years of research have finally yielded a promising lead to the cure for cancer in early 2025: fat cells.
In the lab, it has been commonly understood that obesity increases the risk of developing various types of cancer. Yet recent research indicates that genetically altered fat cells, or adipocytes, may actually be an effective and relatively safe way to combat cancer.
“We believe the engineered cells are outcompeting tumors for essential nutrients, suppressing the proliferation of cancer cells,” Dr. Nahav Ahituv, director of the University of California, San Francisco (UCSF) Institute for Human Genetics, said.
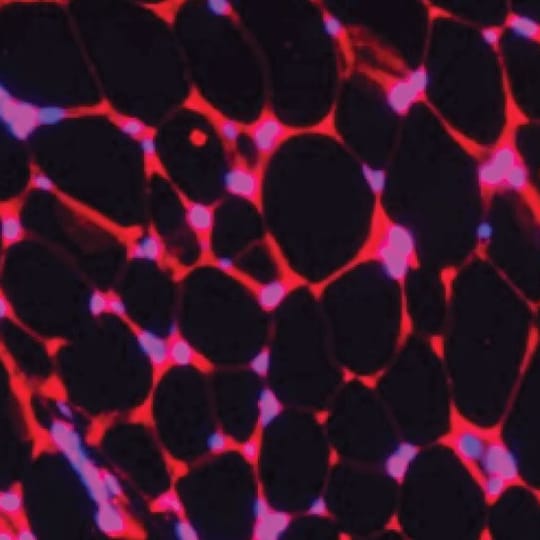
A UCSF research team led by Dr. Ahituv used CRISPR activation, also known as CRISPRa, to express (or increase expression of) a target gene. After observing the behavior of human adipose tissues in different temperatures, Dr. Ahituv and his team began to consider how certain types of fat may interact with cancer. In this study, Dr. Ahituv’s team manipulated specific genes in adipocytes with the intention of causing white adipocytes to act like brown adipocytes.
The primary difference between white and brown adipocytes is energy expenditure, a difference that determines the tissues’ relationship to cancer. White adipocytes store energy while brown adipocytes burn energy to maintain body temperature. Consequently, a surplus of white adipocytes enables many types of cancer to proliferate by increasing levels of fatty acids and specific hormones (e.g., leptin and insulin) in the body, as well as causing inflammation. Brown adipocytes, on the other hand, compete with cancer cells for resources such as glucose and fatty acids.
When the genetically modified adipocytes were implanted in mice with cancerous breast, pancreatic, colon, or prostate growths, Dr. Ahituv’s team observed that tumor growth slowed significantly. This result stayed consistent, no matter where the fat cells were implanted relative to the tumor.
While the effects of the modified adipocytes in humans have not been observed, trials in mice and opportunities for further development highlight the possibility of a new, safe treatment to stop cancer progression.
Compared to existing forms of cancer treatment, such as chemotherapy and surgery, adipose manipulation transplantation (AMT) has thus far proven to be more reliable and less dangerous for patients.
Dr. Ahituv also explains that since liposuction and plastic surgery already remove and replace fat cells, application of AMT is relatively simple and reliable. Although liposuction and plastic surgery may entail side effects such as numbness or imperfectly healed skin, such consequences pale in comparison to the possible ramifications of chemotherapy or invasive surgeries.
“Chemotherapy kills bad cells and good cells in the body,” medical oncologist Dr. Adaeze Iheme said. Killing off “good” (non-cancerous) cells can lead to a weakened immune system, low energy or blood clots, all of which may spiral off into their own complications.
Additionally, surgery is not always a viable option for patients; its efficacy varies depending on how widespread the tumor is or how much it has progressed, barriers that (as of yet) do not seem to apply to AMT.
Yet while bioengineered adipocytes seem the perfect solution on paper, their application in humans, for different types of cancers and their potential side effects still remain to be seen.
“Although AMT aims to starve tumor cells by redirecting nutrient consumption to engineered beige fat cells, it will be important to determine whether this metabolic competition [between the engineered cells and the cancer cells] could also impact normal, healthy cells,” said Dr. Jung Byun, who works in the National Cancer Institute’s Division of Cancer Treatment and Diagnosis.
Even so, experts look towards AMT as a potential cure for cancer in the future rather than merely a tool to halt cancer progression.
“The sky’s the limit for these fat cells,” said Dr. Ahituv.